Non-Val30Met FAP Patients Exhibit Cardiac and Blood Vessel Dysfunction, Study Shows
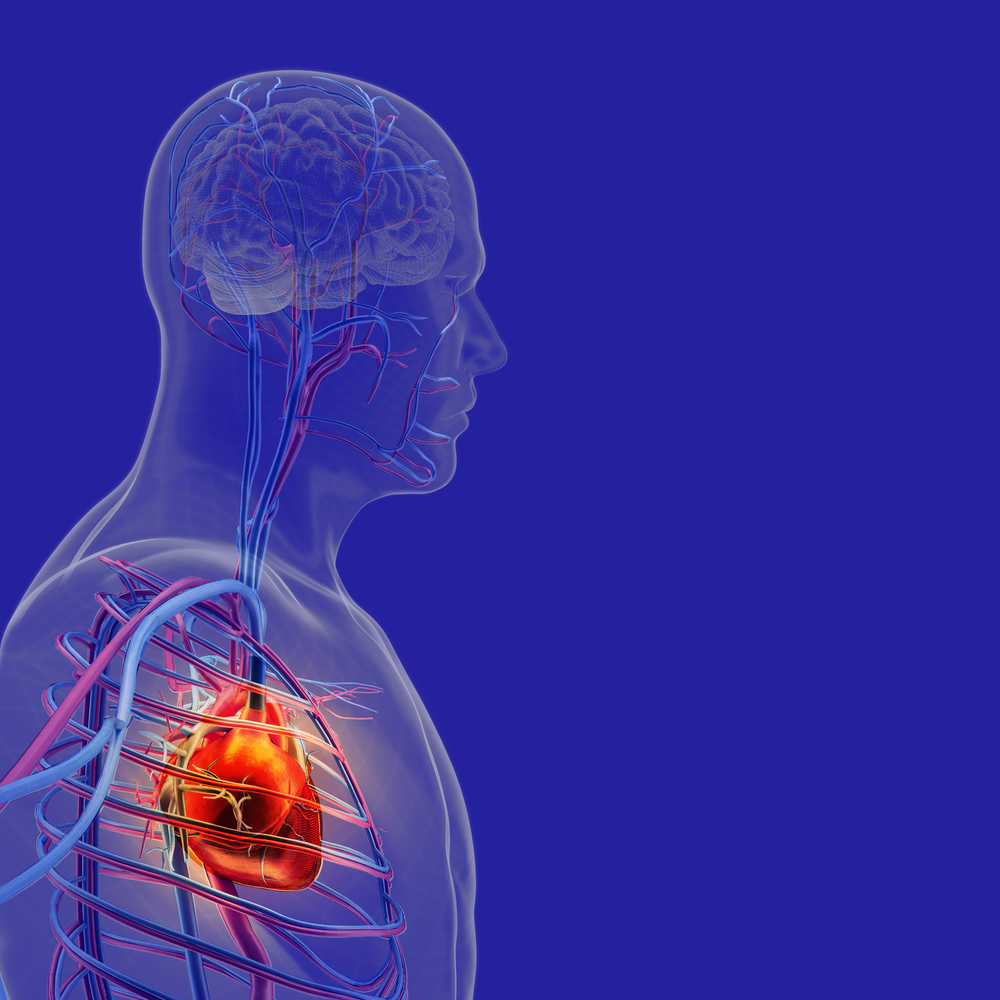
Familial amyloid polyneuropathy (FAP) patients who do not have a Val30Met mutation exhibit prevalent cardiac and blood vessel dysfunction, but proper blood vessel constriction remains intact, even in patients with advanced nerve damage, a study suggests.
The study, “Widespread Cardiac and Vasomotor Autonomic Dysfunction in Non-Val30Met Hereditary Transthyretin Amyloidosis,” was published in the journal J-STAGE.
Familial amyloid polyneuropathy (FAP), also known as hereditary transthyretin (ATTRm) amyloidosis, is a rare progressive disease caused by genetic mutations in the TTR gene, which provides instructions for making a protein called transthyretin.
When genetic mutations occur, the structure of transthyretin changes, preventing it from binding to other transthyretin proteins, a process necessary for its normal transport function. The abnormal TTR protein then starts to form amyloid deposits that accumulate in several tissues, including the nerves, heart, kidneys and eyes, slowly causing damage and eventually giving rise to the symptoms usually associated with FAP.
More than 130 different mutations have been associated with FAP. However, the most frequent mutation — affecting up to 50 percent of FAP patients worldwide — causes one amino acid (the building blocks of proteins) called valine (Val) to be replaced by another called methionine (Met), in position 30 of the TTR gene sequence. This mutation is known as Val30Met.
FAP patients with the Val30Met mutation often exhibit symptoms of autonomic dysfunction early in the course of their disease, and it has been extensively studied in these patients. Autonomic refers to the autonomic nervous system, which is responsible for the control of unconscious body functions such as breathing and heartbeat.
However, autonomic dysfunction in patients with other mutations is not as obvious, and information on how it affects non-Val30met patients is scarce, although some large-scale studies suggest this impairment may commonly occur in these patients.
In this study, researchers aimed to bridge this gap by analyzing the cardiac and peripheral vasomotor autonomic functions of non-Val30Met patients. Vasomotor refers to the dilation or constriction of blood vessels.
Researchers included a total of five patients with different mutations (Val94Gly, Val71Ala, Pro24Ser, Thr60Ala, and Tyr114Cys) who exhibited three major FAP symptoms: neuropathy, cardiomyopathy, and oculoleptomeningeal (eye) involvement.
Participants underwent a series of tests to evaluate their cardiac and vasomotor functions, including the coefficient of variation of R-R intervals (CVR-R), which is a measure of heart function; the Valsalva maneuver, where the patient attempts to forcefully expel air with the nostrils and mouth closed, causing changes in the heart rate and blood pressure; the head-up tilt test, where the patient lies flat on a table and then the upper body is tilted upward in varying degrees to measure changes in blood pressure; the noradrenaline infusion test, in which patients were given a low dose of noradrenaline, a hormone commonly given to restore normal blood pressure; and the (123) I-metaiodobenzylguanidine (MIBG) uptake on myocardial scintigraphy, a diagnostic technique to determine loss of nerve supply to the heart.
The CVR-R, responses to the Valsalva maneuver, and myocardial MIBG uptake all indicated the presence of cardiac sympathetic and parasympathetic dysfunctions in all patients. These are parts of the autonomic nervous system, where the sympathetic system prepares the body for physical and mental activity, while the parasympathetic system is responsible for bodily functions while at rest.
“The profile of cardiovascular autonomic dysfunctions therefore seemed to be similar in our patients regardless of their phenotypes [symptoms presented], suggesting a common pathology of autonomic involvement in non-Val30Met ATTRm amyloidosis,” the authors wrote.
Giving the patients a low dose of noradrenaline caused an increase in systolic blood pressure in all the patients except one with mild neuropathy. This suggests that the patients had an impairment in the function of peripheral sympathetic vasoconstriction, or narrowing of the blood vessels.
“However, the presence of supersensitivity to low-dose noradrenaline suggests that the vasoconstrictor function of the resistance vessels was preserved even in the patient with advanced neuropathy, indicating the usefulness of alpha-adrenoceptor agonists in the management of orthostatic hypotension [drop in blood pressure when standing] in ATTRm amyloidosis patients with non-Val30Met mutations,” the authors said.
These findings indicate that non-Val30Met patients have cardiac and peripheral vasomotor autonomic dysfunctions, but vasoconstrictor function is preserved, even in cases of advanced neuropathy.