Taking a Closer Look at Relationships Between Doctors and Patients

I recently accompanied my husband, Aubrey, to an appointment with a specialist at the hospital and noticed a sign taped to the wall in the waiting room. It was a word cloud graphic highlighting the practices that healthcare practitioners strive for to create a good experience for patients.
As I read it, I felt a sense of recognition and acknowledgement of the specialists, doctors, nurses, pharmacists, and other hospital workers who have been there for my husband throughout his battle with disease.
In 2013, Aubrey, 57, was correctly diagnosed with hereditary ATTR amyloidosis. I mention “correctly” because here in New Zealand, doctors don’t commonly recognize amyloidosis. Patients who have it can go for years without knowing what’s wrong with them. Unfortunately, many families have had to endure loss without knowing what killed their loved ones.
As a wife and a caregiver, my greatest challenge is standing firm while watching Aubrey’s health deteriorate in front of me. In the early stages of his disease progression, I found it incredibly difficult to be left on our own to deal with what we were facing. Due to a lack of amyloidosis experts in the country, those who are diagnosed with it often are told to go home and wait for the next appointment.
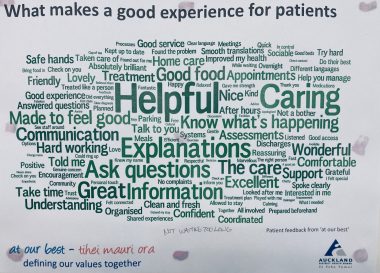
A word cloud graphic made by the Auckland District Health Board in New Zealand hangs on the wall at a local hospital. (Photo by Jaime Christmas)
Which specialists patients are referred to depends on how knowledgeable their primary doctor is, and referrals often can lead to specialists who have little expertise in the disease.
Additionally, every practitioner a patient sees dispenses medication to help with discomfort or pain. But because amyloidosis affects multiple organs in the body, a patient actually needs a team of experts. Aubrey had a squad of specialists at one point, and his list of drugs read like an extended diary. A problem arose when some of the medicines he took interacted with one another and landed him in the hospital.
Admittedly, there was a time when I blamed the doctors and the healthcare system in general for not caring enough and not doing more for the people they serve. When someone is unwell, they depend on their doctor for help to get strong and well again. When the opposite happens, the patient can feel abandoned and disappointed.
But looking at the words highlighted on that picture on the waiting room wall, I realized that everyone involved in disease and caregiving is trying their very best. The ill person just wants to be healthy again to contribute to those around them. Healthcare practitioners are trying to administer the best care for those they serve. I honestly believe that 99.9% of physicians abide by the Hippocratic oath of abstaining from “all intentional wrong-doing and harm.”
In an address to the National Education Association in the U.S. in 1928, physician and surgeon William J. Mayo noted that, “The aim of medicine is to prevent disease and prolong life; the ideal of medicine is to eliminate the need of a physician.”
It may be impossible to eliminate the need for an amyloidosis patient to see a physician, but if both patients and doctors keep doing their best to achieve patient well-being, we can accomplish great things together.
Note: FAP News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of FAP News Today or its parent company, Bionews, and are intended to spark discussion about issues pertaining to familial amyloid polyneuropathy.







Leave a comment
Fill in the required fields to post. Your email address will not be published.