Late-onset FAP Patients Commonly Show Involuntary Nerve and Heart Abnormalities, Study Finds
People with late-onset familial amyloid polyneuropathy (FAP) with the Val30Met mutation in their transthyretin gene commonly have heart and involuntary nerve abnormalities, according to a study published in the Journal of Neurology.
The study, “Cardiac and peripheral vasomotor autonomic functions in late‑onset transthyretin Val30Met familial amyloid polyneuropathy,” aimed to examine the symptoms of late-onset patients from areas where FAP is not common because less is known about these patients.
Earlier studies suggested that such patients may have more symptoms in nerves controlling voluntary actions than in areas where FAP patients are common, who often suffer symptoms related to the loss of autonomic, or involuntary, nerve actions.
Researchers at the Nagoya University Graduate School of Medicine in Japan analyzed eight patients who had been diagnosed with late-onset FAP who were not receiving treatment for their condition. They also included healthy controls to use for comparison.
Most patients had experienced tingling sensations or pain in their arms and legs as their first symptoms.
Examinations revealed that all had some type of heart abnormalities, with enlarged hearts or thickened muscle walls. This did not, however, translate into reduced heart function in any of the study’s patients.
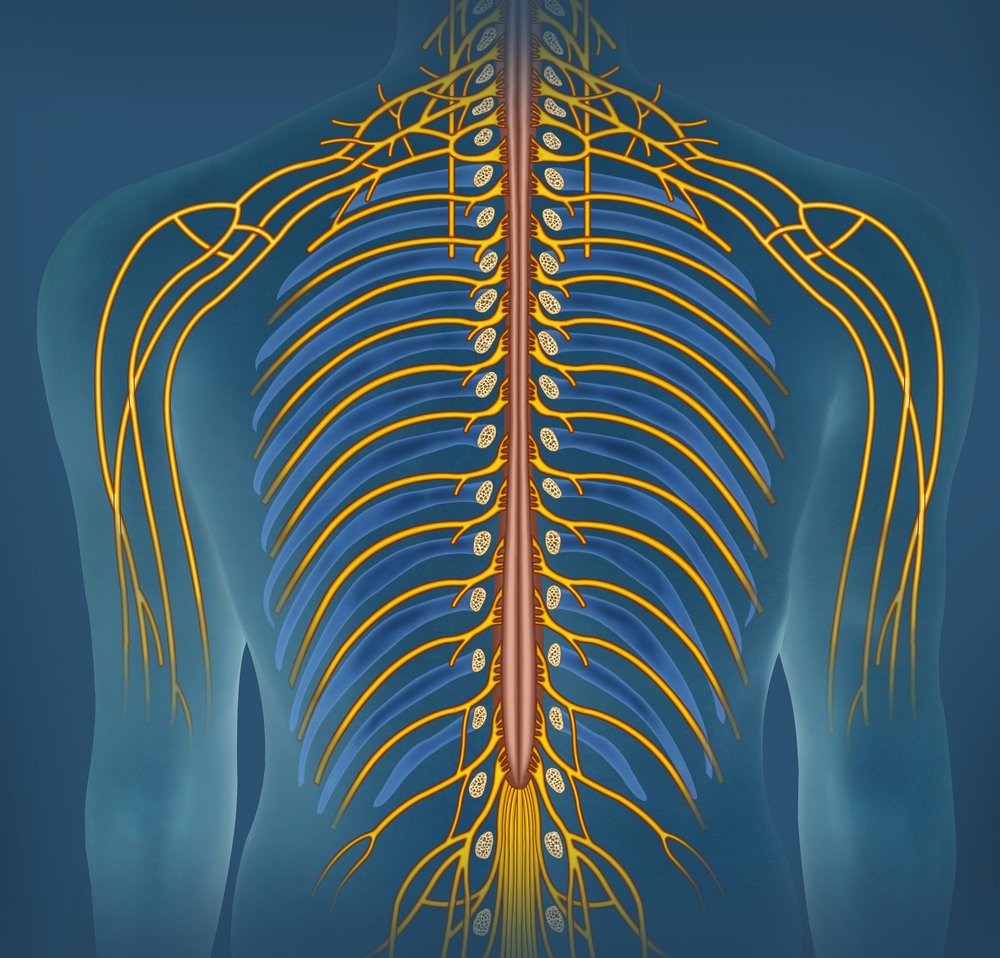
To test the functions of the autonomic nervous system — which guards bodily responses such as blood pressure and gut function — participants went through a range of tests. Orthostatic hypotension, or postural blood pressure drops, can result from the loss of autonomic nerves.
Half the patients showed signs of orthostatic hypotension, which results when nerves that control blood vessel constriction lose their function.
Even though the other half did not show signs of this, they all lacked proper nerve signaling that controls parasympathetic heart function, which is active in situations such as rest or digestion.
The other part of the autonomic nervous system, called the sympathetic system, was also abnormal. This system is known as the “fight or flight” response, and ensures the heart beats stronger and faster when needed. In these patients, the heart did not properly receive such signals.
The team also took a sample of the patients’ sural nerve and noted a loss of fiber density, mainly caused by the lack of myelinated nerve fibers.
They noted that a lack of unmyelinated fibers was more common in patients who had orthostatic hypotension.