Sudoscan noninvasive skin test may help improve early FAP diagnosis
Device to evaluate sweat gland function can assess damage to nerve fibers
Sudoscan, a commercial device that evaluates sweat gland function, might be a useful noninvasive tool to assess damage to small nerve fibers in people with familial amyloid polyneuropathy (FAP), a small study showed.
Those small nerve fibers usually are affected in the early stages of the disease, leading to symptoms like impaired sensation of touch and temperature, as well as neuropathic pain — pain caused by nerve damage, or neuropathy.
Using the Sudoscan likely won’t help in tracking the condition before symptoms start, according to the researchers, but it may aid in evaluating early signs of the disease.
“While the commercial [testing] requires costly equipment, it can automatically analyze [results] in 3 [minutes], making its use applicable in the clinical outpatient setting,” the team wrote.
The study, “Correlation between a commercial electrophysiological test of sudomotor function and intraepidermal nerve fiber density in hereditary transthyretin amyloidosis,” was published in the journal Muscle & Nerve.
Testing the effectiveness of Sudoscan in 39 FAP patients in Japan
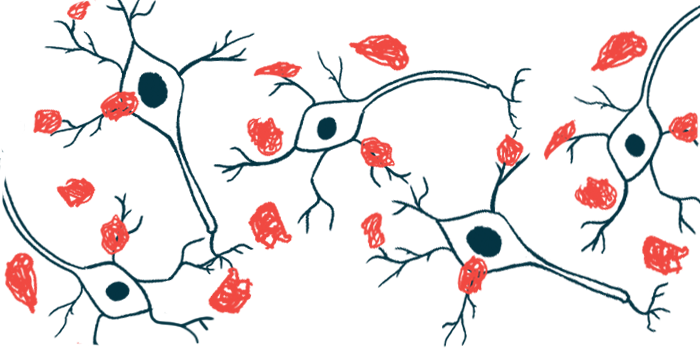
FAP is caused by mutations in the TTR gene that lead to the accumulation of toxic clumps of the transthyretin protein, called amyloid deposits. These deposits mainly occur in the nerves outside the brain and spinal cord, which relay sensory signals.
Small nerve fibers usually are affected first, before large nerve fibers, but the diagnosis of small fiber neuropathy remains a challenge. It commonly relies on a skin biopsy to analyze the density of nerve fibers, which typically is reduced in FAP.
“For early diagnosis of [FAP], the assessment of small fiber neuropathy (SFN) before the appearance of large fiber neuropathy, which leads to abnormal results on nerve conduction studies (NCS), is important,” the researchers wrote. NCS measure the strength and speed at which a nerve can transmit electrical signals.
Getting a correct diagnosis is particularly important, the researchers noted, in light of the recent approvals of disease-modifying therapies that can prevent FAP progression.
Previous studies have suggested that Sudoscan, a commercially available test that’s not invasive, could be used to detect small fiber neuropathy in several diseases marked by this hallmark symptom. The device also may help to distinguish between FAP and other neuropathies.
For early diagnosis of [FAP], the assessment of small fiber neuropathy (SFN) before the appearance of large fiber neuropathy, which leads to abnormal results on nerve conduction studies (NCS), is important.
The test is approved to evaluate sweat gland or sudomotor function in both the hands and feet. It’s based on electrochemical skin conductance (ESC), which measures the release of chloride ions by sweat glands in response to an electrical stimulus. ESC is dependent on the activity of small nerve fibers innervating sweat glands.
Now, researchers in Japan evaluated whether Sudoscan could be used to effectively diagnose small fiber neuropathy in 39 FAP patients in that country. Their study involved 20 men and 19 women with an average age of 51.7.
Besides the most common FAP-causing mutation — V30M, identified in 18 patients — 11 other mutations were found in a smaller number of patients.
Study finds test may be useful in screening and monitoring FAP patients
The most common initial FAP symptom was sensory disturbances in the lower extremities, occurring in 15 patients (38.5%). This was followed by autonomic symptoms — those affecting nerves that control involuntary body functions like breathing or digestion — in nine patients (23.1%).
ESC was categorized as normal, with values higher than 60 microsiemens — a measure of electric conductance — moderately reduced (40-60 microsiemens), and severely reduced (below 40 microsiemens).
The mean ESC was 34.8 microsiemens in the patients’ feet, and 53.8 microsiemens in the hands. Most patients (74.4%) had lower than normal ESC values in their feet, while nearly half (48.9%) had lower ESC in their hands.
The ESC values obtained in the patients’ feet were significantly and moderately associated with the results of all standard neuropathy diagnostic methods evaluated in the study.
These included skin fiber density, as determined in a skin biopsy, nerve conduction tests, clinical scores (neuropathy impairment score and the autonomic section of the Kumamoto Neurologic Scale), and assessment of the heat-related pain threshold.
In the patients’ hands, the ESC values obtained were significantly and moderately correlated with nerve conduction test results, heat-related pain, and the autonomic section of the Kumamoto Neurologic Scale. A weak association was observed with the neuropathy impairment score, while no significant link was detected with skin fiber density.
“In conclusion, our study suggested that [Sudoscan] is a useful noninvasive measurement tool to assess [sudomotor function] via ESC in patients with [FAP],” the researchers wrote.
While Sudoscan may not be effective at detecting amyloid deposits before symptom onset, “the test is non-invasive and easy to perform repeatedly, making it suitable for clinical use in screening and monitoring SFN,” the team added.
Among the study’s limitations, the researchers noted the fact that all included participants were Japanese, which may limit the extension of the study conclusions to other populations.