Small Vesicles in Blood Contribute to Toxic TTR Protein Buildup in FAP

Small vesicles in the blood contribute to the clumping or aggregation, and toxic accumulation of the transthyretin (TTR) protein in people with familial amyloid polyneuropathy (FAP), a study shows.
These findings shed light on the underlying mechanisms of FAP and point to these small blood vesicles, known as extracellular vesicles (EVs), as potential therapeutic targets.
The study, “Extracellular Vesicles Contribute to the Metabolism of Transthyretin Amyloid in Hereditary Transthyretin Amyloidosis,” was published in the journal Frontiers in Molecular Biosciences.
Amyloidosis refers to a group of diseases in which proteins form insoluble clumps, called amyloids, that are deposited outside cells in several organs, causing functional impairment.
FAP is an inherited form of amyloidosis characterized by the toxic accumulation of TTR aggregates due to mutations in the TTR gene. These clumps accumulate mainly in the heart and peripheral nervous system — the network of nerves found outside the brain and spinal cord — leading to heart and neurological damage.
Notably, TTR is mostly produced in the liver, far from the site of its deposits in FAP, and the mechanisms behind its clumping and toxic buildup remain unclear.
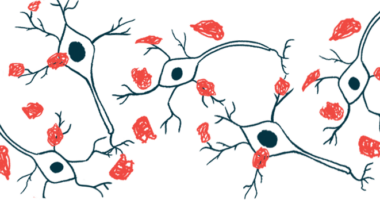
Now, a team of researchers in Japan provided evidence that extracellular vesicles — small fluid-filled sacs — in the blood have an active role in these processes.
Extracellular vesicles are tiny molecule-filled, sac-like structures naturally produced by various cell types in the body to communicate with other cells. Their content often mirrors the state of the cell, and evidence suggests that the release of EVs filled with abnormal or disease-associated proteins may be an early indicator of disease onset or progression.
Researchers first found that TTR was detected in EVs derived from lab-grown liver cells, but not from cells that do not produce TTR. In addition, EVs were necessary for the formation of TTR aggregates in both TTR-producing and TTR-non-producing cells.
Notably, the abnormal TTR protein resulting from the most common FAP-causing mutation, Val30Met, was found to be more prone to bind to blood-derived EVs than the healthy TTR protein, and this binding and aggregation occurred at the surface of EVs.
The team also found that adding both Val30Met-TTR and blood-derived EVs to lab-grown cells significantly increased TTR amyloid deposits around cells and EV uptake by cells, compared with adding each individually.
These findings highlighted that blood EVs promote the clumping and buildup of Val30Met-TTR around cells.
Next, researchers analyzed the blood of six FAP patients — three men and three women — carrying the Val30Met mutation, and six healthy men.
The patients’ ages ranged from 56 to 75, and they had been living with the disease for three to seven years. Blood samples were taken following diagnosis and before treatment start. The age of healthy individuals, who served as controls, ranged from 22 to 40.
The team found that FAP patients showed significantly higher levels of EV markers, but significantly fewer TTR aggregates in blood-derived EVs, relative to controls.
Based on these results, the team hypothesized that in Val30Met-FAP, increased EV numbers and the presence of Val30Met-TTR may increase TTR aggregation in EVs, boost their uptake by cells, and increase TTR deposits in tissues, resulting in a reduction in TTR clumps in blood-derived EVs.
The data suggest that TTR in blood-derived small EVs “is a potential target for future [FAP] diagnosis and therapy,” the researchers wrote.
Notably, several cell membrane proteins are present on the surface of EVs, which may explain the tissue-specific deposits of TTR amyloids outside the liver, the main source of TTR. Further studies are needed to clarify the mechanisms by which EVs contribute to FAP.
Also, given that beta-amyloid — the main protein forming toxic amyloids in Alzheimer’s disease — also builds up in EVs and that TTR is known to suppress the formation of beta-amyloid clumps, “it is necessary to further analyze the relationship between TTR and … EVs derived from the brain, in addition to EVs derived from the liver and other blood sources,” the team wrote.