Echocardiogram for FAP: What to Expect?
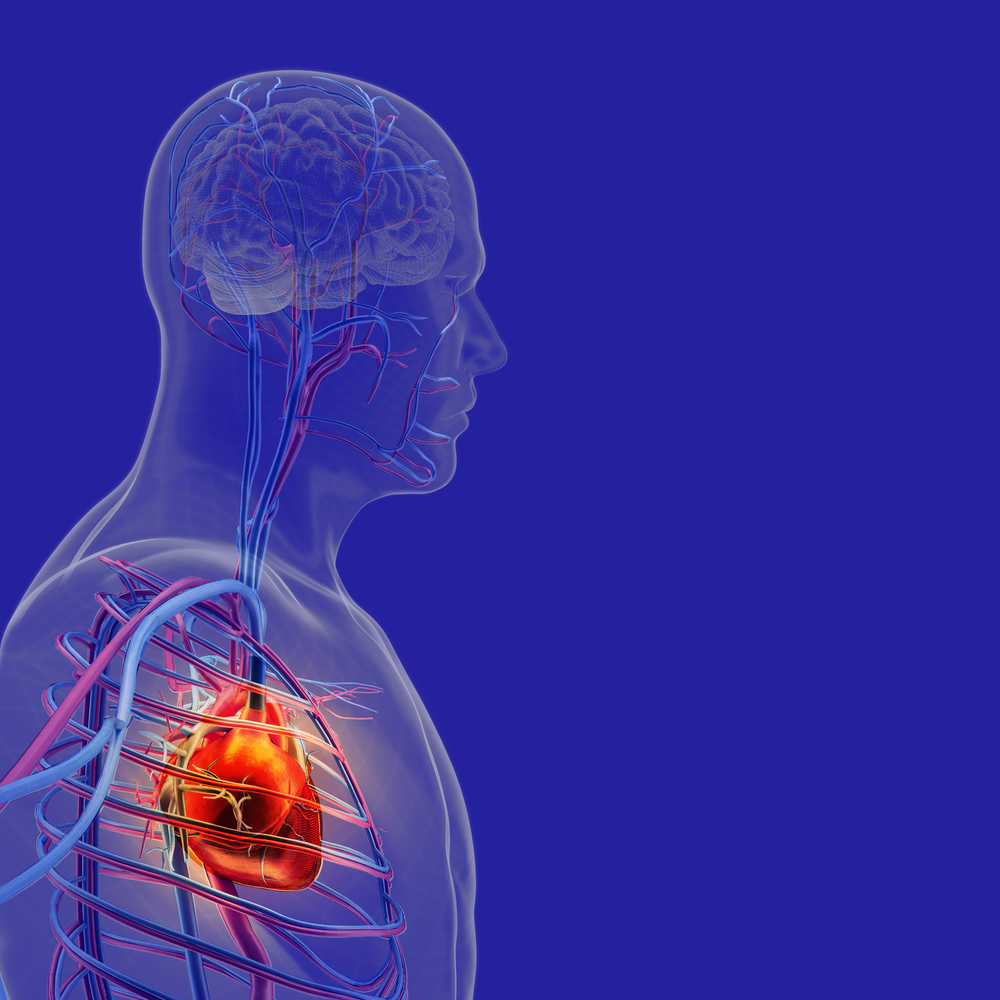
Familial amyloid polyneuropathy (FAP) leads to the formation and accumulation of abnormal protein clumps or amyloids. This accumulation can cause issues in a number of different organs including the heart. Research has shown that around 80% of FAP patients have heart problems. So if you have FAP, your doctor may recommend an echocardiogram to check the health of your heart.
What is an echocardiogram?
An echocardiogram is a test that checks the structure and function of the heart. A machine sends sound waves into your body, which then bounce back. The machine uses the waves that bounce back to construct an image of the heart. In addition to the structure of the heart, the sound waves can show how blood is flowing through the heart.
What are the different types?
Most of the time, your doctor will recommend a transthoracic echocardiogram where the sound transducer is placed on your chest.
If your problems generally only occur when your heart is beating harder or faster, your doctor may recommend a stress echocardiogram. Here, you will undergo testing before and then right after you exercise or receive a medication to increase your heart rate.
Sometimes a contrast agent may be necessary to make some structures, such as the walls of the heart chambers, more visible.
If the doctor is unable to get a clear picture from the surface of your chest, they may need to perform a transesophageal echocardiogram (TEE). Here, they pass the transducer down the throat and into the esophagus. (The esophagus is the tube that connects your mouth to your stomach).
How do I prepare for an echocardiogram?
You don’t need any special preparation before most forms of echocardiogram. You should be able to eat and drink, and take your medications as normal.
If you are undergoing a TEE, your doctor may recommend that you do not eat or drink for eight hours prior to the procedure.
What happens during the procedure?
During the procedure, you will need to remove your clothing from the waist up. You may wear a medical gown.
The doctor or technician may also place electrodes on your chest to record an electrocardiogram, or ECG, at the same time as the echocardiogram.
A doctor or technician will then apply a special gel to a transducer that will be placed on your chest. The gel helps the soundwaves to travel better.
He or she will move the transducer around your chest to record images of different parts of your heart, which will be displayed on a screen. The machine will record the images so that your cardiologist or general physician can view them later.
Your doctor may also use a special technique called Doppler ultrasound to see the direction and speed of the movement of the blood in the heart. The movement will be color-coded on the screen.
If a contrast agent is required, it will be injected into your vein before the procedure.
For a stress echocardiogram, images will be taken first. Then, you will need to increase your heart rate by taking a medication or exercising on a treadmill or stationary bicycle. After your heart rate has increased, a second set of images will be taken.
For TEE, your doctor will give you medication to help you relax. He or she will also numb your throat using a gel or spray. During the procedure, the transducer will be attached to a flexible tube which the doctor will lower down your esophagus and move around to get images of your heart.
What happens after the test?
After the test, you will usually be able to resume your daily activities. If you underwent TEE, you may need to stay in the hospital for observation for a few hours.
The technician will send the images and recordings to your cardiologist or general physician who will meet with you to go over the results.
Last updated: Jan. 21, 2021
***
FAP News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.