Lower Cathepsin E Levels Could Underlie Impaired Function of Macrophages in FAP, Study Suggests
The lower levels of a protein called cathepsin E, upon activation of a type of white blood cells called macrophages, in mice with familial amyloid polyneuropathy (FAP) suggest a role of this protein in cell-mediated immunity. That discovery may help explain the impaired macrophage function in this disease, according to new research.
The study, “Downregulated Cathepsin E expression in bone marrow-derived macrophages from the pre-clinical familial amyloid polyneuropathy model” was published in the journal Amyloid: the Journal of Protein Folding Disorders.
Cathepsin E is mainly produced and active in antigen-presenting immune cells, such as macrophages. Among other functions, previous research from i3S – Instituto de Investigação e Inovação da Universidade do Porto, in Portugal, suggested that cathepsin E could be implicated in macrophages’ chemotaxis (movement in response to chemical signals) in the most severely affected tissues of FAP patients — the peripheral nerves and the gastrointestinal tract.
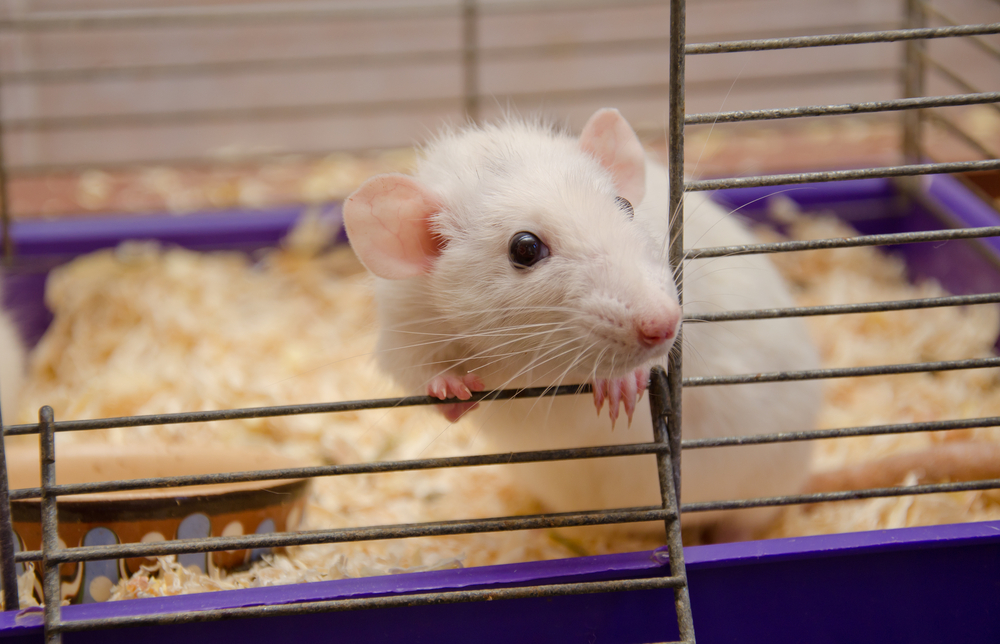
Based on these findings and the reported involvement of macrophages in the clearance of amyloid protein deposits in FAP, as well as in disease progression, the scientists used the TTR V30M transgenic mouse model of the disease to assess the role of cathepsin E in bone marrow-derived macrophages. Of note, TTR V30M is the most common mutation found in FAP patients.
Cells collected from the animals’ femurs and tibia (both leg bones) were seeded into cell culture plates, followed by 24-hour administration of the inflammatory activator LPS to assess the macrophages’ activation and responsiveness.
The results revealed that LPS led to marked cathepsin E reduction in cells from mice with FAP, in comparison to both control cells and FAP cells not exposed to LPS. Of note, cathepsin E production was determined by the levels of messenger RNA, which is derived from DNA in gene expression.
In contrast, no differences were seen in the amount of TNF-alpha, a pro-inflammatory molecule produced by macrophages during acute inflammation.
Taken together with their prior findings, the scientists said these results “could explain the mechanism for lower immune cell chemotaxis and impaired macrophage function observed in FAP.”
Though more studies are needed to unravel the cellular processes, the findings “suggest [cathepsin E] involvement in mediated immunity,” which involves the activation of macrophages, specific antigen-specific T-cells and natural killer cells (a type of lymphocyte).